Understanding Suboxone and Fentanyl
Overview of Suboxone
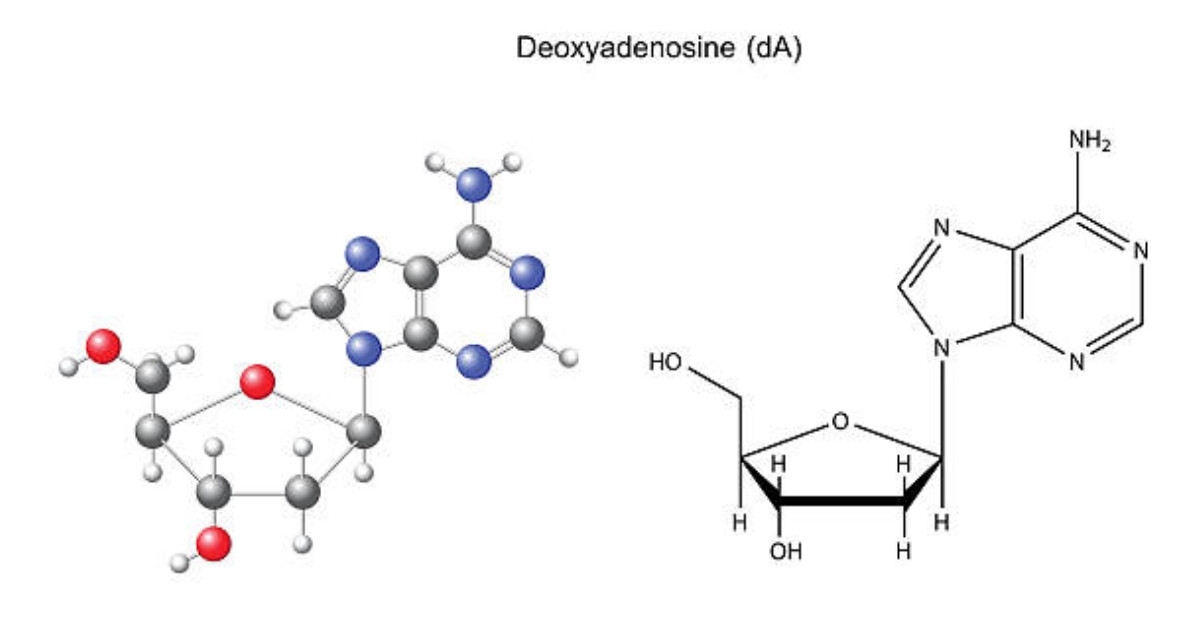
Suboxone is a medication frequently used to treat opioid addiction. It is a combination of two active ingredients: buprenorphine and naloxone. Buprenorphine is a partial agonist that helps alleviate withdrawal symptoms and cravings, while naloxone serves to deter misuse. Suboxone is typically administered as a film or tablet, which dissolves under the tongue.
The goal of Suboxone treatment is to help individuals manage their addiction, facilitating a smoother transition towards recovery. When taken as prescribed, it can significantly lower the risk of relapse for those struggling with opioid dependency.
| Component | Function |
| Buprenorphine | Alleviates withdrawal symptoms and cravings |
| Naloxone | Deters misuse and prevents overdose |
Risks and Dangers of Fentanyl
Fentanyl is a powerful synthetic opioid that is often associated with a high risk of overdose and death. It is estimated to be 50 to 100 times stronger than morphine. Due to its potency, even a small amount of fentanyl can lead to severe respiratory depression, which can be fatal.
The involvement of fentanyl in the opioid crisis has raised significant concerns, particularly because it can be found in counterfeit pills and mixed with other drugs without users’ knowledge. This unpredictability increases the danger for those who consume it.
| Risk Factor | Description |
| Potency | 50 to 100 times stronger than morphine |
| Overdose Risk | High likelihood of fatal respiratory depression |
| Mixed Substances | Often combined with other drugs, increasing danger |
Understanding both Suboxone and fentanyl is crucial for grasping the challenges and potential solutions in addressing opioid dependency. This knowledge helps inform the effects of Suboxone on individuals who use fentanyl and the importance of appropriate treatment options.
The Impact of Suboxone on Fentanyl Consumers
Suboxone is an important tool in the management of opioid dependence, especially for those using fentanyl. The following sections outline how Suboxone works and the potential benefits it offers.
Mechanism of Action
Suboxone is a combination of buprenorphine and naloxone. Buprenorphine is a partial agonist at the opioid receptors, meaning it activates the receptors but to a lesser extent compared to full agonists like fentanyl. This property can help to reduce cravings without producing the same level of euphoria associated with stronger opioids.
Naloxone, on the other hand, is an opioid antagonist. It prevents misuse by blocking the effects of opioids if Suboxone is injected. This dual action makes Suboxone effective in treating opioid dependence.
| Component | Function | Effect on Fentanyl Consumers |
| Buprenorphine | Partial agonist | Reduces cravings and withdrawal symptoms |
| Naloxone | Opioid antagonist | Prevents misuse and mitigates euphoria |
Potential Benefits of Suboxone Use
Suboxone offers several advantages for individuals who use fentanyl. These benefits include:
- Decrease in Opioid Cravings: Many users experience a significant reduction in cravings for opioids, allowing them to focus on recovery and rehabilitation.
- Management of Withdrawal Symptoms: Suboxone helps alleviate the discomfort associated with withdrawal, contributing to a smoother transition during recovery.
- Stability and Functionality: Users of Suboxone often report improved stability in their day-to-day lives, allowing them to engage in work, education, and social activities.
- Lower Risk of Overdose: Due to the partial agonist nature of buprenorphine, there is a theoretically lower risk of overdose compared to using full agonists like fentanyl.
| Benefit | Description |
| Decrease in Opioid Cravings | Helps individuals manage cravings effectively |
| Management of Withdrawal Symptoms | Reduces discomfort during detoxification |
| Stability and Functionality | Enhances daily living and engagement |
| Lower Risk of Overdose | Minimizes the likelihood of fatal overdose |
The use of Suboxone can be a pivotal aspect of treatment for those affected by fentanyl dependency, providing crucial support in their journey toward recovery.
Real-World Effects
Suboxone plays a significant role for individuals who use fentanyl, primarily in managing cravings and withdrawal symptoms. Understanding these real-world effects is crucial for grasping the overall impact of this treatment.
Reduction of Cravings
One of the primary effects of Suboxone is its ability to reduce cravings associated with opioid use, including cravings for fentanyl. The formulation of Suboxone helps to stabilize the individual, making it easier to resist the urge to use.
| Study Context | Percentage Reduction in Cravings |
| Initial Treatment Phase | 74% |
| After 3 Months of Treatment | 85% |
| Long-term Maintenance | 90% |
The data indicates that as individuals progress through treatment, the reduction in cravings can improve significantly, aiding in the recovery journey.
Withdrawal Symptoms and Management
Suboxone also helps in managing withdrawal symptoms that are common among individuals who are dependent on fentanyl. These symptoms can be intense and may include anxiety, insomnia, and physical discomfort. Suboxone mitigates these symptoms, allowing individuals to transition away from fentanyl more comfortably.
| Withdrawal Symptom | Severity Before Suboxone | Severity After Suboxone Initiation |
| Anxiety | High | Moderate |
| Nausea | High | Low |
| Insomnia | Moderate | Low |
| Muscle Pain | High | Moderate |
The table illustrates the decrease in severity of withdrawal symptoms after the initiation of Suboxone treatment, highlighting its effectiveness in managing the challenges faced during recovery.
Suboxone provides substantial benefits for individuals recovering from fentanyl dependence by significantly reducing cravings and alleviating withdrawal symptoms. Understanding these effects is essential for those considering treatment options.
Considerations for Suboxone Treatment
When considering Suboxone treatment for individuals who use fentanyl, several factors must be taken into account to ensure effective and safe recovery. Two critical components of this treatment are medical supervision and individualized treatment plans.
Medical Supervision
Medical supervision is essential when administering Suboxone for treating fentanyl dependence. This oversight helps to monitor the patient’s response to the medication, adjust dosages as necessary, and manage any potential side effects.
| Aspect | Importance |
| Monitoring Health | Regular check-ups for vital signs and overall well-being |
| Dosage Adjustment | Tailoring the dose to maximize effectiveness and minimize risks |
| Managing Side Effects | Addressing any adverse reactions quickly |
| Support System | Providing emotional and psychological support during treatment |
A healthcare professional can offer guidance and ensure that the treatment is progressing positively. This supervision often involves regular appointments and communication between the patient and the provider.
Individualized Treatment Plans
Every individual has unique needs, especially when dealing with substance dependence. An individualized treatment plan considers personal circumstances, history of substance use, and specific health conditions.
| Component | Considerations |
| Personal History | Previous experiences with treatments and substances |
| Co-occurring Disorders | Addressing any mental health conditions alongside substance use |
| Support Systems | Involving family or support groups for enhanced recovery |
| Goals of Treatment | Setting realistic and achievable milestones for recovery |
Creating a tailored plan ensures that the treatment is not only effective but also respects and accommodates each person’s goals and challenges. Individualized approaches can lead to better outcomes and a higher likelihood of sustained recovery.
Challenges and Misconceptions
Addressing the use of Suboxone, several challenges and misconceptions exist, particularly concerning misuse and dependency risks, as well as potential side effects and contraindications.
Misuse and Dependency Risks
While Suboxone serves as a treatment for opioid dependence, there is a risk of misuse. Individuals may take Suboxone outside the prescribed guidelines, affecting its efficacy and leading to new dependency issues.
| Risk Factor | Description |
| Potential for Misuse | Individuals may misuse Suboxone to escape withdrawal symptoms or to experience its euphoric effects. |
| Development of Dependency | Long-term use can lead to physical dependence, resulting in withdrawal symptoms if usage is stopped. |
| Interaction with Other Substances | Combining Suboxone with other substances can heighten risks and lead to dangerous consequences. |
Side Effects and Contraindications
Suboxone is not without side effects. Understanding these effects, as well as contraindications, is vital for individuals considering this treatment. It is essential for healthcare providers to monitor potential side effects.
| Side Effect | Frequency |
| Headaches | Common |
| Nausea | Common |
| Constipation | Common |
| Drowsiness | Less Common |
| Respiratory Issues | Rare |
| Contraindication | Description |
| Hypersensitivity | Individuals allergic to buprenorphine or naloxone should not use Suboxone. |
| Severe Respiratory Issues | Those with severe breathing problems may face heightened risks. |
| Liver Disease | Patients with liver issues require special monitoring as Suboxone is processed in the liver. |
Understanding these challenges and misconceptions allows for more informed discussions around the effects of Suboxone on people who use fentanyl, ensuring safer treatment practices and better outcomes.
Seeking Help and Support
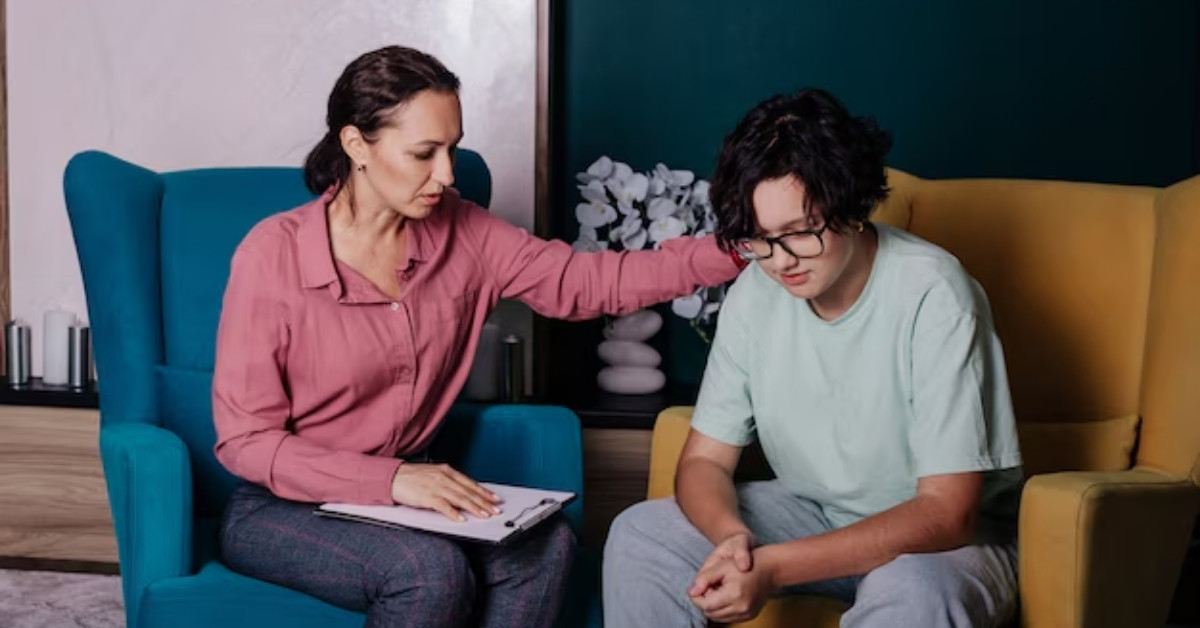
Importance of Seeking Professional Help
Getting professional assistance is crucial for individuals struggling with fentanyl use and considering treatment options like Suboxone. Medical experts can provide guidance tailored to each person’s unique situation, ensuring safety and efficacy throughout the recovery process. Without the right support, individuals may face challenges that hinder their progress, such as severe withdrawal symptoms or relapse.
Medical professionals are trained to understand the complexities of substance use disorders. They can help manage care, monitor progress, and adjust treatment plans as necessary. Engaging with healthcare providers also facilitates access to additional services, such as counseling and support groups, which are essential components of a comprehensive recovery strategy.
Resources for Recovery
Various resources can support individuals in their recovery journey. These resources may include medical facilities, counseling services, support groups, and helplines. Accessibility to these options varies by location but remains critical for effective recovery.
| Resource Type | Description | Examples |
| Medical Facilities | Provide medication-assisted treatment and additional care | Rehabilitation centers |
| Counseling Services | Offer one-on-one therapy to address underlying issues | Individual therapy |
| Support Groups | Facilitate peer support and shared experiences | 12-step programs |
| Helplines | Offer immediate assistance and advice | Crisis hotlines |
Engaging with these resources is vital for individuals seeking to understand the effects of Suboxone on people who use fentanyl. Such support can lead to enhanced outcomes, providing individuals with the tools they need for long-term success.
Sources
https://www.armsacres.com/suboxone-effects-on-people-who-use-fentanyl
https://www.coniferpark.com/effects-of-suboxone-who-use-fentanyl
https://www.wellbrookrecovery.com/suboxone-for-fentanyl-addiction